Osteoporosis is a medical condition characterized by decreased bone mass and density, leading to brittle bones and an increased risk of fractures. It is most common in older adults, particularly women after menopause, but can also affect men and younger people.
Osteoporosis often has no symptoms until a bone fracture occurs, which can occur after a minor fall or even coughing or sneezing. Common fracture sites include the hip, spine, and wrist.
Risk factors for developing osteoporosis include genetics, age, sex, low calcium and vitamin D intake, inactive lifestyle, smoking, excessive alcohol consumption, certain medications such as corticosteroids, and certain medical conditions such as hyperthyroidism and inflammatory bowel disease.
Treatment and prevention of osteoporosis involves a combination of lifestyle modifications, such as increasing calcium and vitamin D intake, weight-bearing exercise, and avoiding smoking and excessive alcohol consumption, as well as medications such as bisphosphonates, hormone therapy, and denosumab. It is important to consult with a health care provider to determine the best treatment plan for individual cases.
Causes
There are many causes of osteoporosis, including:
Age: As people age, their bones tend to become less dense and more fragile.
Gender: Women are at a higher risk of developing osteoporosis than men, particularly after menopause when estrogen levels drop.
Genetics: A family history of osteoporosis increases the risk of developing the condition.
Low intake of calcium and vitamin D: A diet low in calcium and vitamin D can weaken bones.
Inactivity: Lack of weight-bearing exercise can cause bones to weaken over time.
Smoking: Smoking has been linked to decreased bone density.
Excessive alcohol consumption: Excessive alcohol consumption can interfere with the body’s ability to absorb calcium, leading to weaker bones.
Certain medications: Long-term use of certain medications, such as glucocorticoids, can cause bone loss.
Certain medical conditions: Some medical conditions, such as hyperthyroidism, rheumatoid arthritis, and inflammatory bowel disease, can increase the risk of osteoporosis.
It’s important to note that osteoporosis often has multiple causes, and not everyone with the risk factors will develop the condition.
Clinical manifestations
Clinical manifestations of osteoporosis are primarily related to the risk of bone fractures and may include:
Chronic back pain: Osteoporosis can cause chronic back pain due to vertebrae fractures.
Bone fractures: Osteoporosis can increase the risk of bone fractures, especially in the spine, hip, and wrist. Fractures can occur as a result of a minor injury or no apparent injury.
Decreased height: Vertebral fractures can cause a decrease in height.
Postural changes: Bone loss in the spine can lead to a forward curvature of the spine (kyphosis), which is often referred to as a “widow’s hump.”
Bone pain: Some people with osteoporosis may experience bone pain, especially in the hip, wrist, or spine.
It is important to remember that osteoporosis can be asymptomatic until a fracture occurs, so it is important to get screened and follow an appropriate treatment plan if the disease has been diagnosed.
Diagnosis
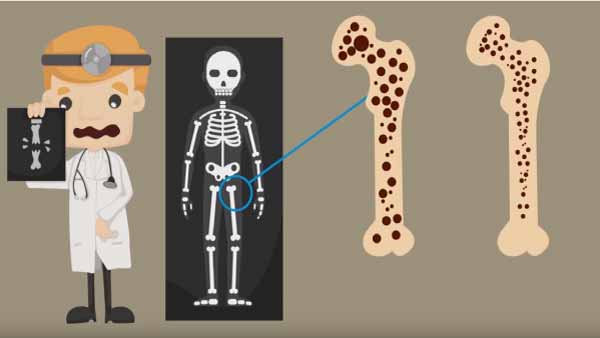
The diagnosis of osteoporosis is made by an assessment of bone mineral density (BMD), which can be measured by bone densitometry. BMD is a measure of the amount of calcium and other minerals in a specific segment of bone, and is used to evaluate bone strength and density.
Bone density is performed in the spine, hip or wrist, and the patient’s bone mineral density is compared with that of a reference population. The results are expressed as a T-score, which compares the patient’s bone mineral density with the maximum bone mineral density found in a healthy young adult. A T-score of -2.5 or lower is considered osteoporosis.
In addition to bone densitometry, laboratory tests may be performed to evaluate the levels of calcium, phosphorus, vitamin D, and thyroid hormones in the blood.
In some cases, additional tests, such as X-rays or CT scans, may be done to detect vertebral fractures or bone abnormalities.
It’s important to talk to a doctor if you have risk factors for osteoporosis, such as a family history of the disease, early menopause, long-term steroid use, smoking, excessive alcohol consumption, or a chronic disease that affects calcium and vitamin D absorption.
Treatments
Treatment of osteoporosis aims to prevent bone fractures and improve bone mineral density. Treatment may include lifestyle changes, nutritional supplements, and medications.
Lifestyle changes: A diet rich in calcium and vitamin D is recommended, along with regular physical exercise for bone health and muscle mass.
Nutritional supplements: They may be recommended for those who did not get enough calcium and vitamin D in their diet. Calcium and vitamin D supplements can help prevent bone loss.
Medications: There are several types of medications available to treat osteoporosis, such as bisphosphonates, teriparatide, denosumab, and raloxifene. These medications can help increase bone mineral density and reduce the risk of fractures.
Hormone therapy: Hormone therapy (HT) may be used in postmenopausal women to prevent bone loss. However, HT is not recommended for all women and can have side effects.
It is important to speak with a doctor to determine the best treatment plan for each individual case of osteoporosis.
Complications
The most common complication of osteoporosis is bone fractures. Fractures can occur in the spine, hip, wrist, and other bones, and can be painful and disabling. Hip fractures, in particular, can have serious consequences, such as increased disability and mortality.
In addition, osteoporosis can lead to decreased mobility and independence, which can have a negative impact on the patient’s quality of life. Osteoporosis has also been shown to be associated with an increased risk of depression.
In severe cases, osteoporosis can lead to permanent deformities and disabilities. Therefore, it is important to take preventive measures and follow a proper treatment plan to prevent serious complications.
Recent research
There is several recent investigations in the field of osteoporosis that focus on identifying new risk factors and improving existing treatments. Some of the most relevant investigations are:
Gene therapy: Gene therapy has been investigated as a possible treatment for osteoporosis. Preliminary studies have shown that gene therapy can improve bone formation and reduce bone loss in mice.
Microbiome: Research has shown that the gut microbiome may be linked to osteoporosis. It has been suggested that changes in microbiome composition may affect bone health and that probiotics may be improvements for osteoporosis prevention.
High-intensity exercise: Studies have shown that high-intensity exercise may be more effective at increasing bone density than low-intensity exercise. This is because high-intensity exercise generates greater load forces on the bones, which can stimulate bone formation.
New drugs: New drugs are being researched for the treatment of osteoporosis. These include therapies that target specific proteins involved in bone formation and resorption, as well as therapies that aim to stimulate bone formation.
Overall, this research is aimed at improving understanding of osteoporosis and finding better treatments to prevent and treat the disease.